Pregnancy is one of the most beautiful times in a woman’s life. But this beautiful time does come with many perks, such as mood swings, dietary changes, health issues and more. Gestational diabetes is one of the problems expected mothers face, even when they have never had diabetes before.
It is still a controversial topic that while few women have gestational diabetes, others do not. One of the vital reasons can be that it is genetic; that is, maybe someone in the family suffers or has had diabetes earlier. Some other noteworthy reasons can be that the mother is overweight before she gets pregnant.
What Is Gestational Diabetes:
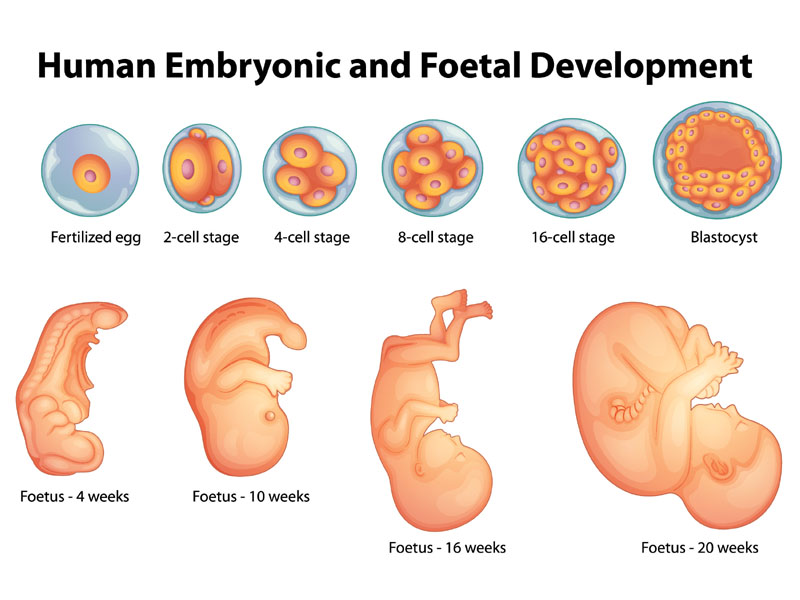
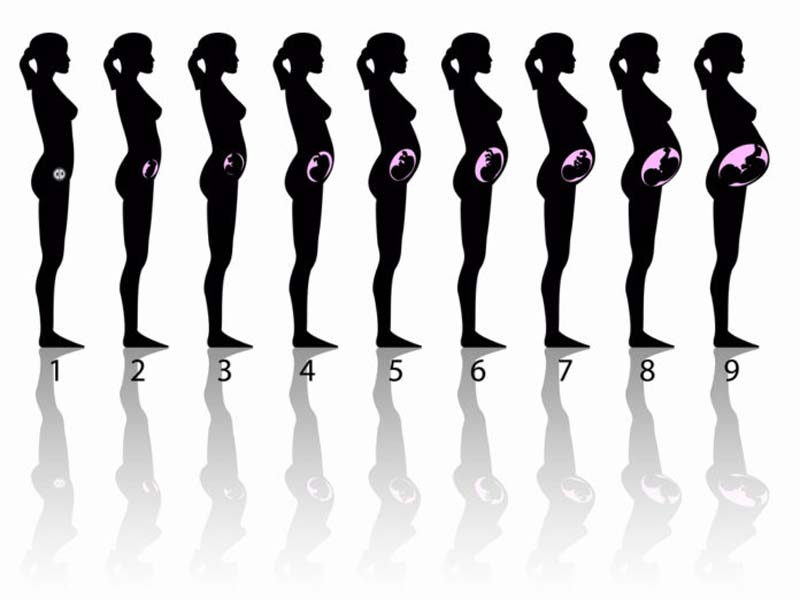
Gestational diabetes is a woman without diabetes who previously developed high blood sugar levels during pregnancy. It affects around 3-9% of pregnancies and is especially common in the last trimester. It occurs due to the several hormonal changes in pregnancy that predispose insulin resistance. (1)
It increases the risk of developing preeclampsia, depression and having a C-section during pregnancy. In 90% of cases, gestational diabetes resolves once the baby is born. However, these women are at a higher risk of developing type 2 diabetes later in life. It affects certain ethnic groups like Asians, American Indians, Indigenous Australians and Pacific Islanders.
See More: Hair Growth During Pregnancy
Cause of Gestational Diabetes During Pregnancy:
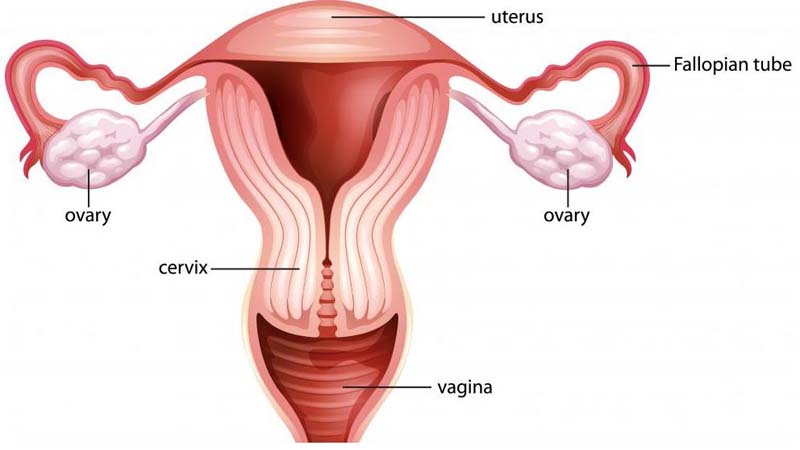
Insulin is a hormone produced by the pancreas that metabolizes glucose into energy. When insulin levels fall, blood sugar levels rise. During pregnancy, the placenta produces hormones which cause a rise in sugar levels. If your body cannot handle this rise in blood glucose by making enough insulin, you get gestational diabetes. It is influenced by genetics and certain other risk factors as well.
Symptoms of Gestational Diabetes During Pregnancy:
Gestational diabetes often has no symptoms or mild ones, such as being thirstier than normal or urinating more. Some of the symptoms are listed below:
- Increased thirst
- Increased fatigue and tiredness
- Excessive hunger
- Increased frequency of urination.
- Frequent urinary tract infections and yeast infections.
- Blurred vision.
Risk Factors for Diabetes in Pregnancy:
You are more likely to develop diabetes during pregnancy if you have the following risk factors. (2)
- Overweight or obese before pregnancy.
- Genetic: If you have a family member with diabetes
- Prediabetes: If you had blood sugars higher than they should be before pregnancy.
- If you have a history of gestational diabetes in previous pregnancies.
- Have other related medical conditions like high blood pressure, etc.
- Fetal macrosomia: If you have given birth to a large baby in previous pregnancies.
- If you have given birth to a stillborn or baby with birth defects in previous pregnancies.
- Older maternal age at conception.
- If you are carrying twins.
- If you have PCOS, acanthosis nigricans or insulin resistance conditions.
See More: Fever During Early Pregnancy
How to Diagnose Gestational Diabetes:
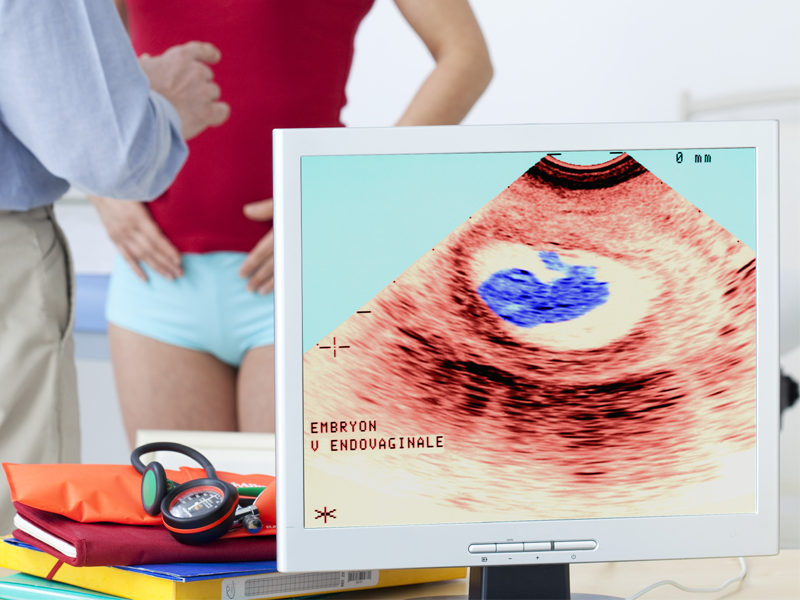
Routine screening occurs at 24-28 weeks of pregnancy or sooner if you have risk factors or a history of diabetes in the family or previous pregnancies.
1. One-step test:
- Your doctor will start by testing your fasting blood sugar levels.
- You will be asked to drink a solution containing 75 grams of glucose.
- Your blood sugar levels will be tested consecutively after one hour and 2 hours.
- You are diagnosed with gestational diabetes if you have any of the following sugar values :
Fasting : > 95 mg/dL
1 hour : > 180 mg/dL
2 hours :> 150 mg/dL
2. Two-step test:
- For the two-step test, fasting is not required.
- You will be asked to drink a solution containing 100 gms of glucose.
- Your blood sugar levels will be tested 1,2 and 3 hours later.
- You will be diagnosed with gestational diabetes if you have any one of the following sugar values :
Fasting : > 95-105 mg/dL
1 hour : > 180-190 mg/dL
2 hours : > 155-165 mg/dL
3 hours : > 140-145 mg/dL.
See More: Low BP During Pregnancy
Treatment of Gestational Diabetes:
If you have been diagnosed with gestational diabetes, your treatment plan will be customized according to your sugar levels.
- Usually, the sugar levels are managed by proper diet, restricting sugar intake, regular exercise, and frequent monitoring of glucose levels.
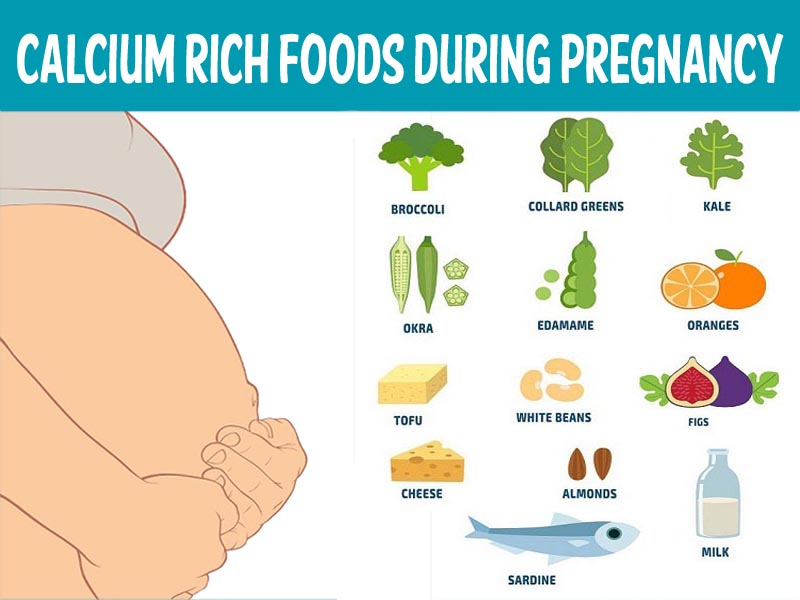
- Healthy diet: It focuses on all the food groups: fruits, vegetables and whole grains, foods that are high in nutrition and low in calories. Limit intake of processed food, sugar foods, preserved foods and drinks. You may want to consult a dietician to create customized meal plans for you according to your blood sugar levels.
- Regular exercise: Regular exercise improves overall well-being and health during pregnancy. It lowers blood sugar levels and increases insulin sensitivity. Exercise also relieves back pain, cramps and general discomfort associated with pregnancy. With your doctor’s consent, aim for a mild workout and include exercises like walking and swimming in your daily routine.
- The next step would be adding a safe oral hypoglycemic drug, approved in pregnancy to reduce sugar levels, coupled with a healthy diet, sugar restriction and regular exercise.
- According to the Mayo Clinic, around 10-20 % of women with gestational diabetes need insulin to help control their sugar levels.
- Along with medication, you are encouraged to monitor your blood sugar levels frequently with a portable handheld glucose monitoring device.
- Your doctor will also inform you about the side effects of insulin injections and tell you what to do if your blood sugar levels fall too low or rise too high!
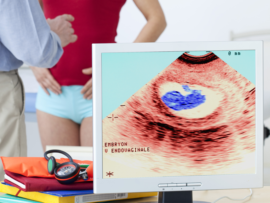
- Close monitoring of your baby: Your doctor might want to closely monitor your baby’s development with repeated ultrasounds or other tests. Post-dated pregnancies with gestational diabetes might increase the risk of complications for you or your baby.
Complications of Gestational Diabetes in Mother and Baby:
If your blood sugar levels are not controlled and are consistently high throughout pregnancy, it can lead to complications and affect the health of your child.
1. Fetal macrosomia: Large baby with high birth weight above 4 kilograms.
2. Neonatal hypoglycemia: Low sugar levels in the baby after birth.
3. Shoulder dystocia due to large baby and difficulty in normal delivery
4. Respiratory distress in the newborn.
5. Preeclampsia: Increased risk of high blood pressure in the mother.
6. C-section: A woman with poorly controlled gestational diabetes is more likely to require a C-section to deliver her baby.
7. Increased risk for babies to develop obesity and type 2 diabetes as adults.
8. Polyhydramnios: Excessive amniotic fluid in the womb can cause premature labour and preterm delivery.
9. Increased incidence of jaundice in the newborn.
10. Increased risk of stillbirth and birth defects.
See More: Vomiting Sensation During Pregnancy
How To Prevent Gestational Diabetes:
- If you are overweight and plan to get pregnant sometime in the future, then you should lower the BMI range to normal with proper diet and exercise. Lowering the BMI can help in preventing gestational diabetes.
- When you are pregnant, visit a doctor during your early pregnancy and make sure that you inform him about any family history of diabetes. Early screening can help in detecting gestational diabetes early.
- You should also stick to a healthy pregnancy diet regardless of what other people tell you and maintain your sugar intake. Craving for sugar is often high in pregnant women, but ensure you do not overindulge in sugar, or it will lead to gestational diabetes.
- After consulting your doctor, a proper exercise routine must be followed to regulate hormonal imbalance and sugar levels.
Even if your diabetes disappears after your baby is born, it is necessary to be careful about diabetes for the next childbirth. You should have your blood sugar levels checked 6-12 weeks after giving birth and once every year after that, even though the results are normal. Some research indicates that a woman with gestational diabetes is at higher risk for developing type 2 diabetes and obesity in later life.
If you have had gestational diabetes before, undergo regular screening and maintain a healthy lifestyle before planning another pregnancy. We hope this article provides information and alleviates all your fears regarding gestational diabetes. Do let us know!!
Frequently Asked Questions and Answers:
Q1. Can gestational diabetes cause miscarriage?
Ans: If a woman has very high uncontrolled blood sugar levels for a prolonged period, it increases the risk of miscarriage. Also, high blood sugar levels in the mother predispose to birth defects, which may cause miscarriages.
Q2. When should we get tested for gestational diabetes during pregnancy?
Ans: Gestational diabetes usually occurs in the second half of the pregnancy. You should get tested between 24-28 weeks or sooner if you are at high risk.
Q3. What are the safe blood sugar levels in pregnant women?
Ans: Fasting blood sugar: < 100 mg/dL
- 1 hour after meals: <140 mg/Dl
- 2 hours after meals: <120 mg/Dl.
Disclaimer: The information provided in this article is for educational purposes only. It is not intended to be construed, or it is a substitute for professional medical advice. If you have signs of gestational diabetes, consult your nearest healthcare provider for diagnosis and treatment.